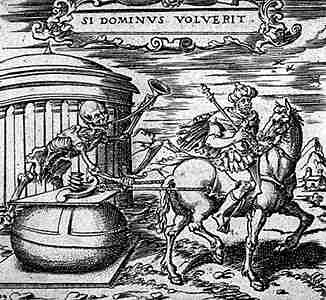
I love this time of year. Time for scary stuff, like
more mad cow disease news, and brand-new Supreme Court
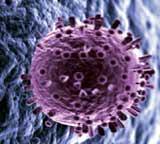
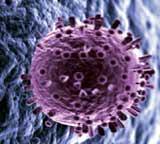
deliberations, and creepy pictures, like this one of a virus penetrating a human cell. That's right, folks, it’s
Pandemic Flu Awareness Week, and that means learning all about how the influenza virus works, what it can do to you when it gets its hemagglutininous hands on your sialic acid receptors, and lastly, getting worried enough to pay attention to what the powers that be
are doing (
or not doing) about it all.
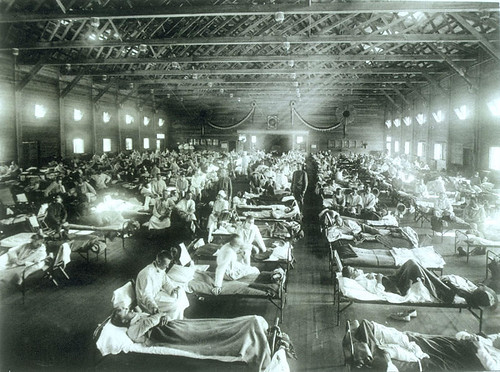
The synchronicity of this is also fairly creepy. Over the last couple years I've been learning about the great flu pandemic of the early 20th century. Just a few years ago PBS ran a documentary about it,
Influenza 1918. Then last week, baited by the Borders' 3 for 2 sale, I picked up a copy of John M. Barry's fine book,
The Great Influenza, an account of the 1918 pandemic of the influenza virus known affectionately among scientists as good old "H1N1". And I've been buttonholing friends and innocent bystanders with all the gory details ever since.

In that exponential way the quest for knowledge expands when a curious reader is exposed to the virus of a fascinating concept, I started reading everything I could find to try to understand what all this was about. I knew something about viruses from the first literary Big Scare, brought on by Richard Preston's
The Hot Zone, which gruesomely detailed the habits and effects of the Ebola and Marburg viruses. What I didn't know was that the 1918 pandemic killed "
more people than any other outbreak of disease in human history," as Barry put it in his book. And it did it in only 2 years' time. The last two days the papers have been full of the latest Bush talking points about how to prepare for a pandemic. Yesterday, as I was working on this post, I heard NPR announcing that a couple teams of
scientists have made a major breakthrough, identifying the 1918 H1N1 killer as a bird flu virus that had jumped species directly into humans. The story has been on the online NYTimes for two days now.

Influenza virus is believed to have originated in wild birds. The one that particularly worries scientists today is known by the catchy name “H5N1”. You've probably heard plenty about this by now: the intermittent reports of
avian flu in Southeast Asia, the slaughter of over a million domestic fowl in
Hong Kong, the deaths of a
Thai woman and her daughter that pointed to a possible first human-to-human transmission, the
surprise deaths in a wealthy Jakarta suburb of a father and his two young daughters who had no known contact with birds.
Why is this so worrisome? While the virus has demonstrated that it can transmit itself bird-to-human, it has not been positively identified as being able to transmit human-to-human (though some circumstantial evidence exists that it may have). And in human-to-human transmission lies the potential for a pandemic. If it establishes itself as a human vector, it can devastate untold numbers of people around the world because, since no such virus has ever attacked the current living human populace, no one now living has developed any immunity to it.
Transmission is a tricky business, because viruses have an almost sci-fi ability to mutate. Most of them are species specific; they may only infect horses and birds, or birds and pigs, or humans and monkeys. Some can adapt to leap the species barrier from, say, bird to human, but once into the new species, cannot go any further. Others, though, can adapt to not only leap that barrier, but settle in and spread throughout the new species, and these adaptations are made possible by genetic mutation. But more on that in a minute.
Yesterday
Bloomberg reported:
“A 23-year-old Indonesian man who died last week tested positive for bird flu, increasing to seven the number of human fatalities from the disease, a doctor at the Sulianto Saroso hospital in Jakarta said.
 The World Health Organization laboratory in Hong Kong will need to confirm the local test results. The UN agency has so far confirmed four human fatalities from H5N1, a deadly strain of the avian influenza virus, in Indonesia....
The World Health Organization laboratory in Hong Kong will need to confirm the local test results. The UN agency has so far confirmed four human fatalities from H5N1, a deadly strain of the avian influenza virus, in Indonesia....
More than 140 million chickens have been slaughtered in Asia because of concern the H5N1 strain of the virus may mutate into a form easily transmissible between humans. As humans are unlikely be immune to such a virus, the World Health Organization is concerned it may trigger an influenza pandemic like the one that led to more than 40 million deaths worldwide in 1918.
The highly pathogenic H5N1 is endemic in poultry in many parts of Indonesia, WHO said in the statement, citing the Food and Agriculture Organization. More than 10 million chickens have been killed by the virus since the outbreak in 2003, Agriculture Minister Anton Apriantono said on Sept. 19.
There has been no confirmation of human-to-human transmission of the virus. One case of probable human-to-human infection occurred in Thailand last year, when a mother and her daughter died from the disease.”
No confirmation. But the more recent deaths in Jakarta
also occurred where no direct contact with fowl was known to have taken place. Let’s take a few steps back, and see what we’re dealing with.
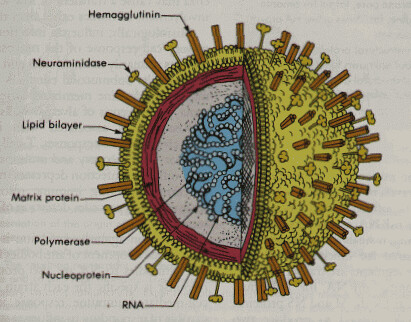
The influenza virus, like all viruses, has only one known function: to replicate itself. It does this by invading a host cell, hijacking the gene-making machinery inside, and forcing the cell to reproduce so many of the original virus that the sheer number of them finally bursts open the cell and kills it. The newly-escaped brood of up to a million new viruses then sets out to do the same to the nearest suitable cells.
What makes a suitable cell? When a bird gets the flu, it goes for the gastrointestinal tract. In human beings, it attacks the respiratory system, which means the
epithelial cells that protect the surface of the lungs and bronchi. (While it may take the virus less than 72 hours to denude the respiratory surfaces of epithelial cells, it will take the body weeks to build them back up again--if it survives). In the meantime, their destruction can allow the virus to penetrate deep into the lobes of the lungs, resulting in viral pneumonia, or let bacteria in, causing bacterial pneumonia. In either case, the resulting war between the invader and the body's immune system can wreak such destruction that, in the worst cases, the capillaries can be destroyed by killer proteins and the lungs fill up with fluid, blood, dead cells, collagen, and fibrin, drowning the victim or causing heart failure or death by exhaustion from the sheer strain of trying to breathe.
Normally when a micro-organism invades the body, the immune system rallies to attack it, and it recognizes the foreign invader by the antigens it carries. Once it has engaged the enemy in combat, the immune system "remembers" what that enemy looks like because the antigens have caused it to release antibodies specific to those antigens. Thereafter, any further attack will rally the same antibodies, resulting in a response so swift and effective that the body can be said to have developed an immunity to the invasive organism. The principle of vaccination capitalizes on this process by introducing antigens into the body in a controlled way so the immune system can learn to recognize them and create the antibodies that will immunize the body in case of future encounters.
The antigens of the influenza virus consist of two types of protrusions carried like spikes all over its surface:
hemagglutinin (the "H" factor), which enables it to bind to the host cell, and once inside, break into the genetic machinery, and
neuraminidase (the "N" factor), which destroys the sialic acid of the host cell and allows the newly-created viruses to escape the dying cell and explode into the body. The flu virus' RNA-based genetic code provides no safeguard against mutation as it replicates in the hijacked cell (resulting in the creation of literally millions of different kinds of "quasi-species" in the course of a few hours), and unlike many other viruses, it can survive the mutation of its antigens and continue to function. Worse, it has the demonic ability to mutate not only properties of these antigens when replicating (antigen drift), but even entirely new antigens if it comes into contact with other different types of flu viruses (antigen shift). "Antigen drift" hides a virus from an immune system that once recognized it, resulting in epidemics, which is why flu vaccines have to be constantly changed and updated. But “antigen shift”, essentially the creation of a brand-new type of virus that the immune system has never encountered in any form, is what causes pandemics, the ultimate concern scientists have about the H5N1 virus. This means if a human being contracts the H5N1 virus from a bird, and also happens to be carrying a human flu virus, the two organisms may collide during replication, where the loose strings of RNA genes may come apart and reassort with each other, suddenly resulting in a virus that inherits the human virus’ ability to transmit from person to person. The same can happen when a 3rd party “mediates” the mutation, as with pigs, which are susceptible to both avian and human viruses. If a pig happens to carry both at the same time, it may pass to its handlers a mutant that may go on to infect other humans.
At this point there is uncertainty as to whether H5N1 has yet mutated in this way, though if it had, its virulence would have likely begun killing far more people by now. The World Health Organization reports that as of 9/29/05, there were
116 cases resulting in 60 deaths--a mortality rate of
52%. But even if the transmission issue is still uncertain, there is absolutely no doubt among scientists everywhere, from those at
WHO to the
Center for Disease Control, that it is a very real danger. The announcement yesterday by the teams of researchers at the CDC confirms that the pandemic flu of 1918 developed just as they fear H5N1 is developing.
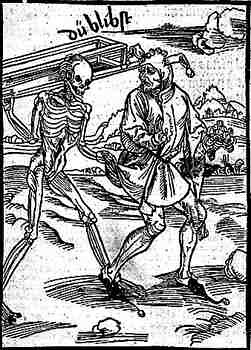
Here is the paradox: the more virulent the influenza virus, the more violently the immune system reacts, and the healthier the immune system is, the stronger that reaction will be. This is why the pandemic of 1918 killed so many young adults. The deaths of young, healthy people in Asia who contracted H5N1 is a warning signal.
What can we do? It's not as if we can get into the lab and whip up our own genetically recombined virus for a vaccine.
Mike Davis, author of
Monster at Our Door, outlined in Common Dreams last year
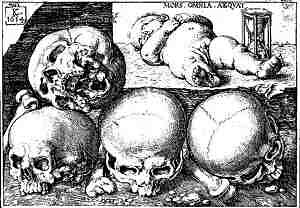
the many problems that would prevent an appropriate and sufficient response to a pandemic: lack of a vaccine and limited production capacity, lack of a vast-enough vaccine delivery system, and lack of public knowledge or interest. Add to that John Barry's more recent assessment: drug-resistant bacteria, insufficient medical facilities, long waiting lists and insufficient manufacturing capacity for antiviral drugs like Tamiflu, massive economic and social disruption, and of course, the deaths, for which current casket inventories would be completely inadequate, resulting in the piling up of corpses in homes and everywhere else.
How many corpses would H5N1 leave in it's wake? Barry's equation is that a new flu virus will make between 14-40% of the population symptomatic. Using that percentage, and using the mortality rate of 52% mentioned above, here in the United States we could expect from 44 million to 115 million to fall ill, and from 23 million to 58 million dead. We have never,
ever experienced that kind of devastation: 20% of our populace dead, and the majority of them, if true to the 1918 virus, young adults.
So now the government has been all over the news the last couple days crowing about all the work they're going to do on this issue.
You saw the Katrina response.
What will you be expecting?
 Here's to the old pagan tradition of wassailing the apple trees. From the Sulgrave Manor website we read:
Here's to the old pagan tradition of wassailing the apple trees. From the Sulgrave Manor website we read: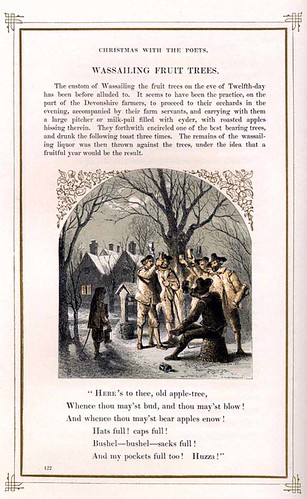 The recipe for making a wassail bowl found in The Joy of Cooking is about as authentic as you can get:
The recipe for making a wassail bowl found in The Joy of Cooking is about as authentic as you can get: While I can't recommend the activity for everyone, I enjoyed it immensely, and although the drink itself wasn't as tasty as I'd hoped for, it was an interesting exercise in reconnecting to the past. But on this, the nub end of the old year and the brink of the new, I can't think of anything better than to wish you all better days and better luck. As the old song says:
While I can't recommend the activity for everyone, I enjoyed it immensely, and although the drink itself wasn't as tasty as I'd hoped for, it was an interesting exercise in reconnecting to the past. But on this, the nub end of the old year and the brink of the new, I can't think of anything better than to wish you all better days and better luck. As the old song says:






 I wish I could say I'll miss NOLA, or Louisiana, but I won't. It's too flat for my soul, and I miss the seasons. Fall doesn't exist here, at least in a way that makes sense to a Yankee. The few Halloween decorations I've noticed look as out of place as a Christmas tree in the middle of a bandstand on a summer night. But most of all, I won't miss the constant low-level misery, the endless fighting back against despair that is the lot of every person here. I've come to love the strength, humor, and compassion of the local people. But I don't have enough of any of those qualities to bear their miseries."
I wish I could say I'll miss NOLA, or Louisiana, but I won't. It's too flat for my soul, and I miss the seasons. Fall doesn't exist here, at least in a way that makes sense to a Yankee. The few Halloween decorations I've noticed look as out of place as a Christmas tree in the middle of a bandstand on a summer night. But most of all, I won't miss the constant low-level misery, the endless fighting back against despair that is the lot of every person here. I've come to love the strength, humor, and compassion of the local people. But I don't have enough of any of those qualities to bear their miseries."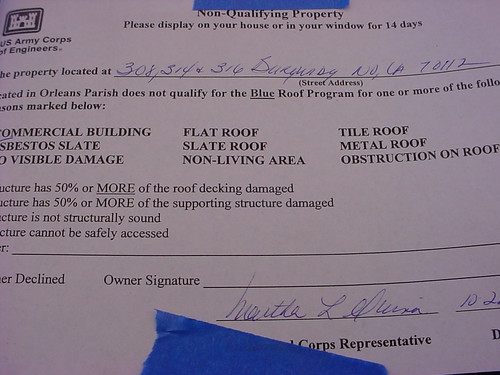



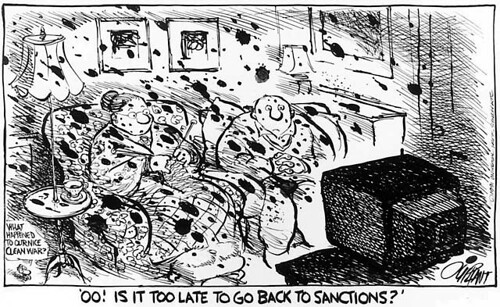
 I'm not adding one more voice to the chorus, however well intended, about how brave and heroic the warrior class is. Because what it comes down to is that you put people out there in endlessly repeated situations where all that matters is staying alive and depending on their comrades to help them do that, and then you praise them for it. You pick out the inevitable shining diamonds of decency and the moments of humanity that many of them act out, that will let them rise above the carnage for however brief a moment, and praise them and what they have had to endure, and it makes the attraction of fighting and dying all the more alluring, cements the mythology even more tightly to the reality it obscures, the reality that war is death to the human soul and a wallow in the worst evils man can produce. The young are full of fire and believe in their own immortality and are eager to prove to themselves and the world that they can walk through that fire, and the old are eager to give them the chance by stoking them with
I'm not adding one more voice to the chorus, however well intended, about how brave and heroic the warrior class is. Because what it comes down to is that you put people out there in endlessly repeated situations where all that matters is staying alive and depending on their comrades to help them do that, and then you praise them for it. You pick out the inevitable shining diamonds of decency and the moments of humanity that many of them act out, that will let them rise above the carnage for however brief a moment, and praise them and what they have had to endure, and it makes the attraction of fighting and dying all the more alluring, cements the mythology even more tightly to the reality it obscures, the reality that war is death to the human soul and a wallow in the worst evils man can produce. The young are full of fire and believe in their own immortality and are eager to prove to themselves and the world that they can walk through that fire, and the old are eager to give them the chance by stoking them with  A
A 








 I love this time of year. Time for scary stuff, like
I love this time of year. Time for scary stuff, like 
 Influenza virus is believed to have originated in wild birds. The one that particularly worries scientists today is known by the catchy name “H5N1”. You've probably heard plenty about this by now: the intermittent reports of
Influenza virus is believed to have originated in wild birds. The one that particularly worries scientists today is known by the catchy name “H5N1”. You've probably heard plenty about this by now: the intermittent reports of 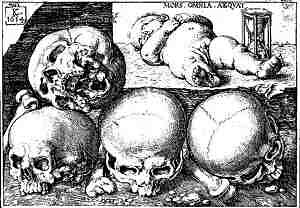 Transmission is a tricky business, because viruses have an almost sci-fi ability to mutate. Most of them are species specific; they may only infect horses and birds, or birds and pigs, or humans and monkeys. Some can adapt to leap the species barrier from, say, bird to human, but once into the new species, cannot go any further. Others, though, can adapt to not only leap that barrier, but settle in and spread throughout the new species, and these adaptations are made possible by genetic mutation. But more on that in a minute.
Transmission is a tricky business, because viruses have an almost sci-fi ability to mutate. Most of them are species specific; they may only infect horses and birds, or birds and pigs, or humans and monkeys. Some can adapt to leap the species barrier from, say, bird to human, but once into the new species, cannot go any further. Others, though, can adapt to not only leap that barrier, but settle in and spread throughout the new species, and these adaptations are made possible by genetic mutation. But more on that in a minute. The World Health Organization laboratory in Hong Kong will need to confirm the local test results. The UN agency has so far confirmed four human fatalities from H5N1, a deadly strain of the avian influenza virus, in Indonesia....
The World Health Organization laboratory in Hong Kong will need to confirm the local test results. The UN agency has so far confirmed four human fatalities from H5N1, a deadly strain of the avian influenza virus, in Indonesia....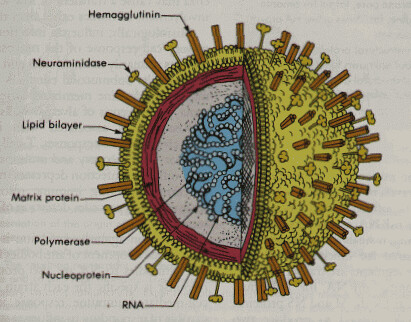 The influenza virus, like all viruses, has only one known function: to replicate itself. It does this by invading a host cell, hijacking the gene-making machinery inside, and forcing the cell to reproduce so many of the original virus that the sheer number of them finally bursts open the cell and kills it. The newly-escaped brood of up to a million new viruses then sets out to do the same to the nearest suitable cells.
The influenza virus, like all viruses, has only one known function: to replicate itself. It does this by invading a host cell, hijacking the gene-making machinery inside, and forcing the cell to reproduce so many of the original virus that the sheer number of them finally bursts open the cell and kills it. The newly-escaped brood of up to a million new viruses then sets out to do the same to the nearest suitable cells.
 The antigens of the influenza virus consist of two types of protrusions carried like spikes all over its surface:
The antigens of the influenza virus consist of two types of protrusions carried like spikes all over its surface:  At this point there is uncertainty as to whether H5N1 has yet mutated in this way, though if it had, its virulence would have likely begun killing far more people by now. The World Health Organization reports that as of 9/29/05, there were
At this point there is uncertainty as to whether H5N1 has yet mutated in this way, though if it had, its virulence would have likely begun killing far more people by now. The World Health Organization reports that as of 9/29/05, there were 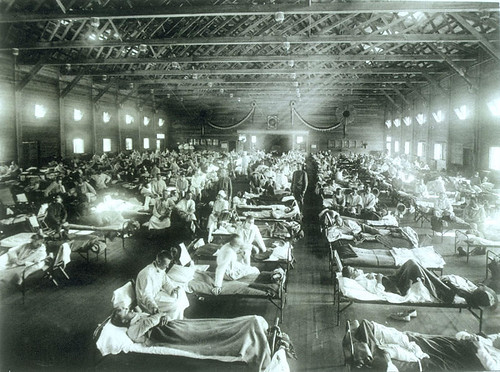 What can we do? It's not as if we can get into the lab and whip up our own genetically recombined virus for a vaccine.
What can we do? It's not as if we can get into the lab and whip up our own genetically recombined virus for a vaccine.  There's just no point in commenting on something as self-evident as
There's just no point in commenting on something as self-evident as 
 Paul William Roberts' book,
Paul William Roberts' book,  According to
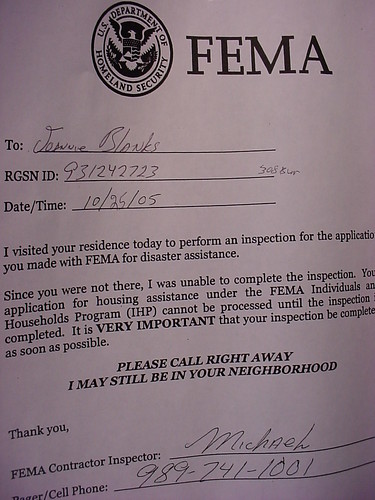
According to  Yesterday I spent all day in an expedited training in preparation to go south to do
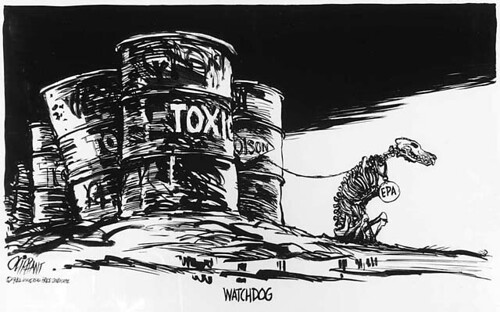
Yesterday I spent all day in an expedited training in preparation to go south to do  Pat Oliphant is the premiere editorial cartoonist living today. His work combines classic draftsmanship, beauty and mastery of medium with a powerfully keen sardonic edge and an unmatched ability to marry symbols to issues.
Pat Oliphant is the premiere editorial cartoonist living today. His work combines classic draftsmanship, beauty and mastery of medium with a powerfully keen sardonic edge and an unmatched ability to marry symbols to issues.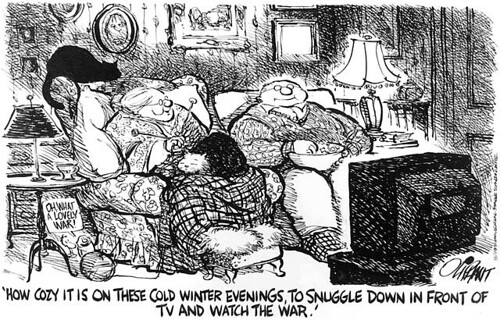
 It’s been a few days since the anti-war march in D.C., and by now there are some excellent write-ups about it out there, especially from
It’s been a few days since the anti-war march in D.C., and by now there are some excellent write-ups about it out there, especially from  We headed up Pennsylvania Ave. and stopped at the Old Post Office for a break, where we discovered the American flag is considered a dangerous weapon. “No flags!” barked the guard, and one of us had to stay outside with the arsenal, while the rest of us had to empty our pockets and remove our traitorous buttons before we were allowed to proceed to the venerable inner sanctum, which, while lovely, still bore a suspicious resemblance to your local yuppie galleria.
We headed up Pennsylvania Ave. and stopped at the Old Post Office for a break, where we discovered the American flag is considered a dangerous weapon. “No flags!” barked the guard, and one of us had to stay outside with the arsenal, while the rest of us had to empty our pockets and remove our traitorous buttons before we were allowed to proceed to the venerable inner sanctum, which, while lovely, still bore a suspicious resemblance to your local yuppie galleria. Even then the crowd, nearly elbow to elbow, was so huge we couldn’t see anything except what stuck up above our heads. Although the march was supposed to start at noon, we stood there for 2 more hours as the crowd grew and surged around us, absorbing more and more people, clueless as to why we couldn’t get started. It was only later that we realized the crowd had become so big that they couldn’t fit us all onto 15th Street.
Even then the crowd, nearly elbow to elbow, was so huge we couldn’t see anything except what stuck up above our heads. Although the march was supposed to start at noon, we stood there for 2 more hours as the crowd grew and surged around us, absorbing more and more people, clueless as to why we couldn’t get started. It was only later that we realized the crowd had become so big that they couldn’t fit us all onto 15th Street. We watched the grassy area around the Washington Monument fill in with people. (The Monument, by the way, has glowing, blinking red eyes that glare down at you while the 1st Air Cav or something buzzes around it like a biplane trying to distract King Kong.) The speakers’ area and tents were only about half a city block away from us, yet the effort to fight our way through to get to them was so great that most of us decided to stay put, while Robin and her husband sallied forth to get the full technicolor experience.
We watched the grassy area around the Washington Monument fill in with people. (The Monument, by the way, has glowing, blinking red eyes that glare down at you while the 1st Air Cav or something buzzes around it like a biplane trying to distract King Kong.) The speakers’ area and tents were only about half a city block away from us, yet the effort to fight our way through to get to them was so great that most of us decided to stay put, while Robin and her husband sallied forth to get the full technicolor experience. A guy in a George Bush mask on a tricycle with a backpack PA, welcoming us to his parade. When the crowd did finally start to move, it was extremely slow and intermittent. It took almost two hours to get from 15th Street to the White House in peristaltic contractions, working our way through the streets like a large meal through a python’s guts. Old people wore “Bush is a Moron” t-shirts. Babies wore buttons telling us to ask them about the Downing Street Memo. Songs and chants birthed and died in our throats along the way.
A guy in a George Bush mask on a tricycle with a backpack PA, welcoming us to his parade. When the crowd did finally start to move, it was extremely slow and intermittent. It took almost two hours to get from 15th Street to the White House in peristaltic contractions, working our way through the streets like a large meal through a python’s guts. Old people wore “Bush is a Moron” t-shirts. Babies wore buttons telling us to ask them about the Downing Street Memo. Songs and chants birthed and died in our throats along the way. In spite of the tight quarters and forced intimacy, in spite of stepping on toes and shoving flagpoles into each other’s faces, in spite of the usual problems that arise in any enormous crowd, the feeling was mellow. People were gentle with each other, and patient, and the only anger I saw was directed at the murderers in the government. Regardless of the scowling, screaming youths in the few photos run by the media, there was none of that anywhere within our sphere. People were enjoying themselves, and welcoming each other, and tolerating each other.
In spite of the tight quarters and forced intimacy, in spite of stepping on toes and shoving flagpoles into each other’s faces, in spite of the usual problems that arise in any enormous crowd, the feeling was mellow. People were gentle with each other, and patient, and the only anger I saw was directed at the murderers in the government. Regardless of the scowling, screaming youths in the few photos run by the media, there was none of that anywhere within our sphere. People were enjoying themselves, and welcoming each other, and tolerating each other.  The atmosphere was festive, like a fair or a carnival, and it was exhilarating to be with others who shared our goal. It was a constant high, being with them and feeding off their excitement. It was always about ending the war. I never, ever felt the anti-war message was lost or watered down. Only near 4:30, at the very end of the march, did a group of youngsters come drumming down the street chanting about Palestine. By then things were breaking up. We were heading for the train. Their appearance seemed like an afterthought, and about as important.
The atmosphere was festive, like a fair or a carnival, and it was exhilarating to be with others who shared our goal. It was a constant high, being with them and feeding off their excitement. It was always about ending the war. I never, ever felt the anti-war message was lost or watered down. Only near 4:30, at the very end of the march, did a group of youngsters come drumming down the street chanting about Palestine. By then things were breaking up. We were heading for the train. Their appearance seemed like an afterthought, and about as important. Marching in Washington D.C. on September 24 was the best thing I could have done that day, and I’m proud to have been there, and proud to have contributed to it, and I don’t give a shit what anyone else thinks. I’m sick of reading the broadsides against the organizing and the sponsors, the marginalization of the event, the trivializing of the numbers who attended, and the wailing about how this is no way to get the Democratic machine to get on board because that’s the only way to end the war, world without end, amen.
Marching in Washington D.C. on September 24 was the best thing I could have done that day, and I’m proud to have been there, and proud to have contributed to it, and I don’t give a shit what anyone else thinks. I’m sick of reading the broadsides against the organizing and the sponsors, the marginalization of the event, the trivializing of the numbers who attended, and the wailing about how this is no way to get the Democratic machine to get on board because that’s the only way to end the war, world without end, amen. Anyone who looks at the march and says it didn’t matter because no one important was on board doesn't know how to measure importance. They want a leader, a Martin Luther King, to get up and speak at these things, but where do they propose we find such a one? Not one person, outside of Robert Byrd, can match that kind of eloquence, and the left holds its nose at Byrd because of his white-robed past. They say the message was too diffuse, but they weren't there to be able to say exactly
Anyone who looks at the march and says it didn’t matter because no one important was on board doesn't know how to measure importance. They want a leader, a Martin Luther King, to get up and speak at these things, but where do they propose we find such a one? Not one person, outside of Robert Byrd, can match that kind of eloquence, and the left holds its nose at Byrd because of his white-robed past. They say the message was too diffuse, but they weren't there to be able to say exactly  Anyone who says there was too much theatre there on Saturday, or the people behind it were too wacky, or the wackjobs ennabled the media to make it a joke, or one march isn’t going to change anything, needs to stop whining and fingerpointing, get off their ass, and show us some blueprints: what's your big idea for turning the country around? What have you done so far, other than type out your disapproval for the efforts of others? Let's have it, and let's hear what you yourselves are doing to make changes, and then maybe I'll listen. Till then, I'll do what I think is important for others, and what is life-affirming for me. Because declaiming in H.L. Mencken tones about the crappiness of it all is good for blowing off steam for awhile, but it doesn't do a damned thing to make things better. (And yes, I'm both inside and outside the system, working on multiple levels to bring positive change to my community and to the nation and the wider world as well. Just in case you wondered. And even if you didn't.)
Anyone who says there was too much theatre there on Saturday, or the people behind it were too wacky, or the wackjobs ennabled the media to make it a joke, or one march isn’t going to change anything, needs to stop whining and fingerpointing, get off their ass, and show us some blueprints: what's your big idea for turning the country around? What have you done so far, other than type out your disapproval for the efforts of others? Let's have it, and let's hear what you yourselves are doing to make changes, and then maybe I'll listen. Till then, I'll do what I think is important for others, and what is life-affirming for me. Because declaiming in H.L. Mencken tones about the crappiness of it all is good for blowing off steam for awhile, but it doesn't do a damned thing to make things better. (And yes, I'm both inside and outside the system, working on multiple levels to bring positive change to my community and to the nation and the wider world as well. Just in case you wondered. And even if you didn't.)